Syphilis
Outbreak Training Website
The Clinical Stages of Syphilis | what type of illness can you get with syphilis?
Syphilis (Treponema pallidum subsp. pallidum) is associated with different clinical stages although approximately 50% of people infected have no symptoms. The required treatment will vary depending on the progression and stage of the syphilis infection and local/jurisdictional guidelines (below).
|
Jurisdictional guidelines for syphilis testing and clinical management protocols |
|
|
Jurisdiction |
Title of Guideline (including website link) |
|
National |
Syphilis Series of National Guidelines (SoNG), Developed by CDNA and updated in August 2018, provides nationally consistent guidelines for public health units in responding to syphilis. |
|
Pregnancy care guidelines within SoNG: Syphilis Chapter of the Pregnancy Care Guidelines In addition, the updated in 2019, includes strengthened recommendations for testing females during pregnancy. |
|
|
Western Australia |
|
|
Northern Territory |
|
|
Queensland |
Communicable Diseases Control Guidance and Information : A-Z |
|
South Australia |
South Australian STI Guidelines Aboriginal Health Council of South Australia STI BBV handbook |
WARNING: This section contains images of genitalia and medical procedures. It is recommended for ages 18+.
Note: the following signs and symptoms may or may not be present in syphilis all cases. Syphilis signs and symptoms vary from client to client, with some clients being asymptomatic at all stages.
A sore (or chancre) may occur at the site of infection, 9 to 90 days (average of 21 days) after transmission. Chancres are typically painless, 1–2 cm diameter, single or a few sores (sometimes on a part of the body that curves) with associated painless lymphadenopathy (swollen lymph nodes). Usually, chancres heal rapidly with treatment, and without treatment will heal spontaneously in 3 to 8 weeks and may still be present in up to a third of people at the onset of secondary syphilis symptoms.
A secondary infection, for example with a streptococcal or staphylococcal bacterial infection, can occur, where the chancre may be weeping and very tender with erythema (redness) and swelling around the ulcer, and tender localised lymphadenopathy (swollen lymph nodes). Secondary infections of chancres can be mistaken for genital herpes. If secondary infection is present, it is best to treat the superficial bacterial infection as well as the syphilis infection.
Primary syphilis presentation summary:
- Chancre (sore): painless, 1-2 cm diameter, single or few sores
- Appears at site of infection 9-90 days afterwards
- Resolves spontaneously 3- 8 weeks post infection
- Can still be present in people presenting with secondary syphilis
- Swollen lymph nodes
- In conjunction with bacterial infection: chancre can be weeping and tender – treat bacterial infection as well
|
Stages of syphilis |
Duration of infection from initial contact |
Treatment |
Infectiousness |
|
Primary syphilis |
< 2 years |
Treat with benzathine benzylpenicillin injection 2.4 million units (1.8 gm) IM stat |
Still infectious |
Image credit: Melbourne Sexual Health Centre STI Atlas
Image credit: Melbourne Sexual Health Centre STI Atlas
General primary syphilis
 Oral chancre
Oral chancre
Men's Business
 Penile chancre
Penile chancre 
Women's Business
 Vulvar chancre
Vulvar chancre
Note: the following signs and symptoms may or may not be present in syphilis cases. Syphilis signs and symptoms vary from client to client, with some clients being asymptomatic at all stages.
If left untreated, syphilis enters a secondary stage marked by a range of signs and symptoms that can come and go over 12 months. With treatment, symptoms resolve rapidly. Without treatment symptoms will spontaneously resolve within 2 years.
Some common secondary syphilis presentations include:
A rash – commonly maculo-papular (small raised red bumps) but can vary
- Moist flat patches on mucosal membranes (condylomata lata) in the genital and groin areas, or moist papules (bumps), mucous patches or ulcers in the mouth
- Systemic symptoms such as low-grade fever, malaise (generally feeling unwell), headache, muscle aches and pains, lymphadenopathy (swollen lymph nodes)
- Maculopapular (small bumpy rash) or a scaly psoriatic type (dried skin) rash on the body involving palms and soles
- Patchy hair loss of the scalp and eyebrows
|
Stages of syphilis |
Duration of infection from initial contact |
Treatment |
Infectiousness |
|
Early Secondary |
< 2 years |
Benzathine benzylpenicillin injection 2.4 million units (1.8 gm) IM stat |
Still infectious |
Image credit: Melbourne Sexual Health Centre STI Atlas
General primary syphilis

 Rash on palms
Rash on palms



Rash on soles - third image resembling psoriasis

 Facial skin lesion
Facial skin lesion
 Nodular rash and patchy alopecia
Nodular rash and patchy alopecia

 Typical rash on upper body
Typical rash on upper body
 Rash on back
Rash on back

 Oral lesions
Oral lesions
Men's Business - secondary syphilis



Syphilitis penile balanitis (rash)
 Scrotum balanitis (rash)
Scrotum balanitis (rash)
Women's Business - secondary syphilis
 Multiple painful indurated vulvar ulcers
Multiple painful indurated vulvar ulcers
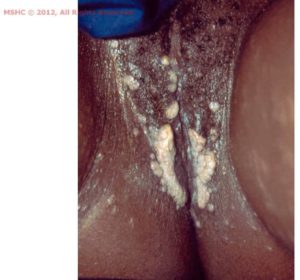 Vulvar condylomata lata
Vulvar condylomata lata

 condylomata lata
condylomata lata
Note: the following signs and symptoms may or may not be present in syphilis cases. Syphilis signs and symptoms vary from client to client, with some clients being asymptomatic at all stages.
Latent syphilis is the description used when there may be no signs and symptoms and the infection is detected and classified by a blood test.
While most sexual transmission occurs during primary, secondary syphilis and early latent syphilis, transmission from mother to baby can occur during pregnancy via blood up to 9 years after the initial infection (latent syphilis). Treatment of latent syphilis differs depending on whether it was acquired within the previous 2 years (early latent) or more than two years ago (late latent syphilis).
|
Stages of latency |
Duration of infection from initial contact |
Treatment |
Infectiousness |
|
Early Latent |
< 2 years |
Treat with benzathine benzylpenicillin injection 2.4 million units (1.8 gm) IM stat |
Still infectious |
|
Late Latent |
> 2 years |
Weekly for 3 weeks Treat with benzathine benzylpenicillin injection 2.4 million units (1.8 gm) IM stat Treatment is very important to prevent long-term consequences. |
No longer infectious
|
Note: the following signs and symptoms may or may not be present in syphilis cases. Syphilis signs and symptoms vary from client to client, with some clients being asymptomatic at all stages.
Tertiary syphilis can cause bone, cardiovascular and neurological changes in up to one third of untreated people at least 7 years after the initial infection. Tertiary syphilis is now rare due to effective treatment and the widespread use of antibiotics. It can occur more rapidly in people co-infected with Human Immunodeficiency Virus (HIV).
The diagnosis of tertiary syphilis is difficult and should always be done in consultation with an appropriate specialist.
Note: the following signs and symptoms may or may not be present in syphilis cases. Syphilis signs and symptoms vary from client to client, with some clients being asymptomatic at all stages.
Congenital syphilis is a syphilis infection affecting a baby in the uterus or newborn. Syphilis can be transmitted from mother to baby during pregnancy and delivery. Transmission is extremely high in early infectious syphilis (90-100% transmission in primary or secondary syphilis) and decreases over time but can still occur many years after the initial infection. How syphilis affects the baby depends on at what stage the mother was infected and therefore at what stage in pregnancy it is transmitted.
Poor outcomes associated with congenital syphilis include:
· mid-term miscarriage,
· death in utero,
· stillbirth,
· bone and organ damage,
· blindness.
Congenital syphilis refers to a range of abnormalities and manifestations which may or may not be evident at birth. Babies infected in late pregnancy or delivery, may have no clinical abnormalities evident at birth but will likely present with congenital syphilis within the first few years of life if not managed appropriately at birth.
The diagnosis of congenital syphilis is difficult and should always be done in consultation with an appropriate specialist.
Image Credit: Centres for Disease Control and Prevention
Image Credit: Centres for Disease Control and Prevention
 Mucous patches
Mucous patches
 Perforation of palate
Perforation of palate
 Hutchinson teeth in infant (https://www.healthline.com/health/hutchinson-teeth#causes)
Hutchinson teeth in infant (https://www.healthline.com/health/hutchinson-teeth#causes)
 Mulberry Molars (https://dentagama.com/news/what-are-mulberry-molar-teeth)
Mulberry Molars (https://dentagama.com/news/what-are-mulberry-molar-teeth)
