Syphilis
Outbreak Training Website
While not replicating the above guidelines, the following information aims to highlight some of the key information regarding the natural history, testing, and management of syphilis.
Why Testing for Syphilis is Important
Prompt and appropriate testing and management of syphilis is essential to:
- Prevent the ongoing transmission to sexual partners
- Prevent the transmission from mother to baby and subsequent poor outcomes such as miscarriage, stillbirth, and congenital syphilis
- Prevent illness caused by syphilis, including secondary and tertiary syphilis
- Reduce transmission of HIV and other STIs and blood-borne viruses (BBVs), which cause genital sores or inflammation of the mucous membranes
Who and When to Test for Syphilis
Health practitioners (Aboriginal and Torres Strait Islander Health Workers and Practitioners, midwives, doctors and nurses) should consider the need for syphilis testing as much as possible and provide treatment for people presenting with any signs or symptoms that could be due to syphilis or other STIs and BBVs.
Syphilis testing should be repeated frequently for those at highest risk.
Refer to the Syphilis Series of National Guidelines (SoNG) for Public Health Units for a list of high-risk groups and the STI/HIV Testing Guidelines for MSM (STIGMA) for additional information.
|
Priority populations for syphilis testing |
|
|
Testing for syphilis should always be included when conducting a check-up for STIs and BBVs and when any other STI or BBV has been detected as co-infections are common. |
|
|
Men who have sex with men (MSM) |
|
|
Priority populations defined by age, sexual orientation and/or location |
During an outbreak situation screen at least 6 monthly Priority populations: remote areas, young Aboriginal and Torres Strait Islander people aged 15–40 years, women of childbearing age Note: age groups and frequency depend on the jurisdiction and local guidelines should be used |
|
People who are pregnant |
Recommend testing at:*
*See local guidelines for further information, particularly in an outbreak declared area, as recommendations for repeat testing vary. If there is a clinical suspicion of syphilis or exposure to syphilis, refer to syphilis guidelines and seek urgent specialist advice. |
|
HIV positive people |
Tested up to 4 times a year for syphilis Routine CD4+ and viral load testing should be done at the same time if clinically appropriate |
|
People who have previously been treated for syphilis |
Once reactive, the syphilis antibody screening test will remain positive for life, but this does not protect against re-infection of syphilis. Syphilis serology should continue to be tested as per local/state/national epidemiology and guidelines |
|
Symptomatic presentation Test for syphilis when someone of any age presents with any signs and symptoms possibly due to syphilis or other STIs and BBVs such as: |
|
|
Asymptomatic Screening Asymptomatic screening for syphilis should be done routinely in the following circumstances:
|
|
Syphilis in pregnancy
Infectious syphilis in pregnancy requires an urgent response and treatment and follow up commenced as soon as possible and within 24 hours.
- Seek advice from an expert in sexual health or infectious diseases regarding the care of females who test positive and their partners.
- In areas affected by an outbreak, treat females with symptoms of syphilis or a new positive PoCT as soon as possible without waiting for confirmatory testing, particularly if there is a risk of loss to follow-up.
- For females with newly confirmed infectious syphilis, give intramuscular 2,400,000 units (given as two 1,200,000 units injections) benzathine penicillin as soon as possible, ensuring that females receive treatment at least 30 days before the estimated date of birth to ensure adequate treatment before the birth.
Ensure contact tracing (including offering testing and treatment to identified contacts) is carried out. Involve an expert in contact tracing if required or seek advice from a sexual health or other relevant expert.
For people with penicillin hypersensitivity (allergies to penicillin), there are two alternative therapies for treatment:
- Desensitisation to penicillin: only penicillin is effective in pregnancy, those allergic should be desensitised then treated with penicillin. Seek specialist advice.
- Non-penicillin regimes: while there is less evidence than penicillin, doxycycline has been shown to be effective; seek specialist advice.
Testing for syphilis: treponemal and non-treponemal testing
There are two types of syphilis testing. Treponemal tests are specific to syphilis but only tell us if someone has ever had syphilis (including an old infection that has already been treated). Non-treponemal tests tell us information about how infectious the person is and how recent the infection is likely to be. We use both types of testing to screen and diagnosis syphilis.
Syphilis testing: false positive test result
A false positive is when the test results come back as positive, but the patient is actually negative for the infection.
False positive test results can occur with:
- both treponemal and RPR tests.
- False positive treponemal tests may be identified in the laboratory as an unclear or indeterminate test result but confirmatory tests are usually conducted with another treponemal test before the result is reported as reactive or non-reactive.
The RPR test is read manually and therefore results may vary slightly among specimens taken at different times or processed at different laboratories. Biological false positive results can also occur with the RPR for a number of reasons including acute infections, inflammation, injecting drug use and pregnancy. False positive RPR results should only cause a low titre reading (usually <1:8) while laboratory errors or variations are generally only within 1 titre of each other. Reactive RPR results should always be considered as true positives among people at risk and an increase in RPR of two titres from the previous RPR considered a likely new infection.
Syphilis testing: false negative test result
A false negative is when the test results come back as negative, but the patient is actually positive for the infection.
False negative test results can occur among people who have:
- Very early syphilis and are tested before the test is measurable in the blood
- A prozone reaction where a large antibody (immune) response can make the test falsely negative
- Immune-suppression due to HIV or other causes.
If there are any concerns about possible false positive results among people at low risk of infection, or false negative results among people likely to have syphilis always contact the regional PHU or appropriate specialists for advice and repeat testing.
Clinical Management | Follow-up and other considerations
Clinical management recommendations during an outbreak
To improve treatment of infectious syphilis, the Syphilis SoNG emphasises the importance of prompt and appropriate management of cases and contacts which support the existing state and national STI management guidelines and include the following recommendations:
- Treatment should be given at the time of presentation to people presenting with signs or symptoms of primary or secondary syphilis.
- Treatment of infectious syphilis identified on serology should be given as soon as possible and ideally within 2 days.
- A serum specimen for syphilis serology RPR should be taken to give a baseline on the day of treatment (even if most recent test was the day before)
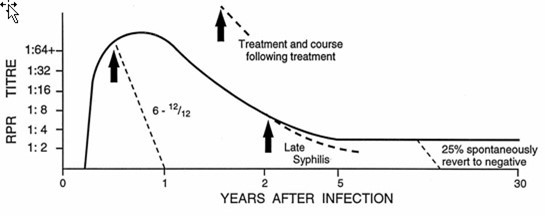
- The RPR on the day of treatment is necessary to show the RPR falling at 3-6 months and 12 months (or in accordance with local guidelines) demonstrating that treatment is working.
- Follow-up RPR testing should be done by the same laboratory as the RPR done on the day of treatment.
- Increased follow-up in an outbreak situation is helpful to look for re-infection where contact tracing has not been possible by the patient not disclosing their partners, or re-infection in a much higher prevalence situation.
- Jarisch-Herxheimer reaction is a common reaction to treatment in patients with primary and secondary syphilis. It occurs six to 12 hours after commencing treatment and is an unpleasant reaction of varying severity with fever, headache, general feeling of being unwell, body shakes and joint pains, which can last for several hours. Symptoms are controlled with pain medicines and rest. Patients should be made aware that this reaction may occur and reassured accordingly.
Follow up
- Follow up serology to check for response to treatment should be done at 3, 6 and 12 months. A two titre (four-fold) drop indicates an adequate response to treatment at 6 months. Local guidelines should be used to ensure frequency is correct according to the jurisdiction.
- Once reactive, the syphilis antibody PoCT test will remain positive for life, but this does not protect against re-infection of syphilis. Syphilis serology should continue to be tested as per sexual risk factors and local epidemiology and guidelines.
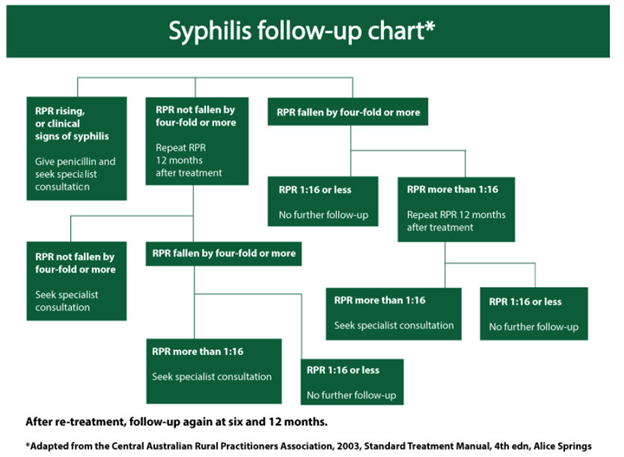
Follow up chart: https://ww2.health.wa.gov.au/Silver-book/Notifiable-infections/Syphilis
WA clinicians please note
Structured Administration and Supply Arrangement’s (SASA’s)
The Structured Administration and Supply Arrangements (SASAs) for Treatment of Syphilis Infection by Registered Nurses and Aboriginal Health Practitioners enable the administration of antibiotics for treatment of syphilis in WA. The SASA’s, and associated Conditions for administering treatment, were developed in consultation with public health physicians from WA Department of Health, WA Country Health Service and Aboriginal Community Controlled Health Organisations, and consultant sexual health physicians.
Please click on the links below to read the relevant SASA:
SASA - Treatment of Syphilis Infection by Aboriginal Health Practitioners
SASA - Treatment of Syphilis Infection by Registered Nurses
Other STI and HIV testing
As STIs and BBVs are often acquired together, it is important to check these when testing for syphilis. The tests required will depend on your patient’s gender, symptoms and whether there are any abnormal findings on physical examination. Refer to your local guidelines for more information.